Our Patient-Centric Approach to Treatment
Georgia Ophthalmologists believes treating each person as an individual is an essential part of each patient’s #VisionForLife.
How is is diagnosed?
Keratoconus is commonly diagnosed through a comprehensive eye exam conducted by an eye doctor or ophthalmologist. If keratoconus is suspected, additional tests such as corneal topography may be advised to provide detailed cornea imaging.
-
Visual Acuity Test
This test measures how well you can see at various distances, both with and without corrective lenses.
-
Refraction Test
The prescription test measures nearsightedness, farsightedness, and astigmatism to determine proper corrective lenses.
-
Corneal Topography
Computer imaging maps corneal curvature and identifies irregularities, aiding in diagnosing vision conditions.
-
Still-Lamp Examination
This test involves the use of a special microscope to examine the surface of the cornea in detail.
-
Pachymetry
A specialized microscope is used to examine the corneal surface during this diagnostic test meticulously.
-
Keratometry
Keratometry measures corneal curvature, aiding in determining appropriate vision correction.

The Georgia Ophthalmologists Approach
Dr. Bigles is a highly experienced refractive cataract surgeon with a successful track record of performing advanced cataract procedures, offering patients improved vision and quality of life. Meanwhile, Dr. Pace is an associate surgeon in the practice, who trained under Dr. Bigles’ guidance, and is known for his dedication to delivering compassionate care and achieving excellent surgical outcomes for patients with cataract conditions.
Call us for a free consultation.

Patients Say
What are the symptoms?
The symptoms of keratoconus can vary from person to person and may include:
- Blurred or distorted vision
- Sensitivity to light
- Halos or ghosting
- Eye strain
- Frequent changes in prescription
- Eye rubbing
See an eye doctor if you experience any of these symptoms, as keratoconus can progress and lead to severe vision loss if left untreated.
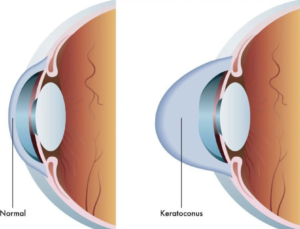
What causes keratoconus?
The exact cause of keratoconus is not fully understood, but it is thought to be a combination of genetic and environmental factors. Some of the factors that have been associated with the development of keratoconus include:
- Genetics
Evidence suggests that keratoconus can run in families, and certain genes may be associated with an increased risk of developing the condition. - Eye Rubbing
Frequent rubbing of the eyes can cause thinning and wearing of the cornea, which may contribute to developing keratoconus - Connective Tissue Disorders
Keratoconus has been linked to certain connective tissue disorders, such as Ehler-Danlos and Marfan syndrom - Chronic Eye Irritation
Chronic eye irritation, such as from poorly fitting contact lenses or allergies, may contribute to developing keratoconus - UV Light Exposure
Some studies have suggested that excessive exposure to UV light may be a risk factor for keratoconus
It is important to note that not everyone with these risk factors will develop keratoconus; some people without any of them may still develop the condition.
What are the treatment options?
The treatment options for keratoconus depend on the severity of the condition and may include the following:
Eyeglasses: In the early stages of keratoconus, eyeglasses may be sufficient to correct vision problems. However, as the condition progresses, glasses may not be able to provide adequate vision correction.
Contact lenses: Scleral fitted contact lenses, or Rigid gas permeable contact lenses (RGPs), are often used to treat keratoconus. These lenses are designed to fit over the cone-shaped cornea, providing a smoother surface for light to enter the eye.
Corneal cross-linking: This minimally invasive procedure involves applying a special solution to the cornea and exposing it to ultraviolet light. This helps to strengthen the cornea and slow or stop the progression of keratoconus.
Intacs: This surgical procedure involves placing small plastic rings in the cornea to reshape it and improve vision. Intacs are typically used for mild to moderate cases of keratoconus.
Corneal transplant: A corneal transplant may be necessary in severe cases of keratoconus where other treatments are ineffective. This involves replacing the damaged cornea with a healthy cornea from a donor.
Combination therapy: Sometimes, combination treatments may be recommended to achieve the best possible vision correction.
Working with an eye doctor who is experienced in treating keratoconus is essential to determine the best treatment approach for your needs.
What is iLink Corneal Cross-Linking?
iLink corneal cross-linking is the only FDA-approved procedure in the United States and is used to treat progressive keratoconus, a condition in which the cornea thins and bulges. During iLink corneal cross-linking, riboflavin eye drops are applied to the cornea, followed by exposure to ultraviolet light.
This combination helps strengthen the cornea by creating new cross-links between collagen fibers, which can halt or slow the progression of keratoconus.
Dr. Jose Bigles
Dr. Jose Bigles is a fellowship-trained refractive surgeon experienced in treating a wide variety of ophthalmic disorders, and specializes in restoring vision through iLink corneal cross-linking treatment for keratoconus. Contact our office to schedule an examination!
For more information about Keratoconus visit Living With Keratoconus
LEARN MOREFAQ
-
How long will the procedure take?
This painless procedure takes approximately one hour to complete. Most of this time is spent applying eye drops and delivering UV light to the cornea.
-
Is it safe?
It is a highly safe procedure with benefits that last a lifetime.
-
Can the iLink procedure reverse keratoconus?
The iLink corneal cross-linking procedure can only halt its progression, which is why early diagnosis and treatment are critically important.
-
What should I expect post-op from the iLink procedure?
After the iLink procedure, patients should expect some discomfort on the corneal surface for which eye drops and oral medications are prescribed.
-
Does insurance cover iLink corneal cross-linking?
The medical necessity of FDA-approved iLink corneal cross-linking has become widely recognized. As a result, the procedure is covered by over 95% of commercial insurance providers. For additional information on insurance coverage and to view the latest list of insurers with policies that cover cross-linking, visit the Insurance Information page on LivingwithKeratoconus.com
Vision For Your Lifestyle
SURVEY FOR CATARACT PATIENTS
You have an important decision to make about your vision future. This survey is designed to help us understand your vision goals so we can provide you with the best possible lens for your lifestyle.
-
General Contact info@georgiavisioncare.com
Contact an Office
-
Phone (770) 786-1234
Fax(770) 385-0813